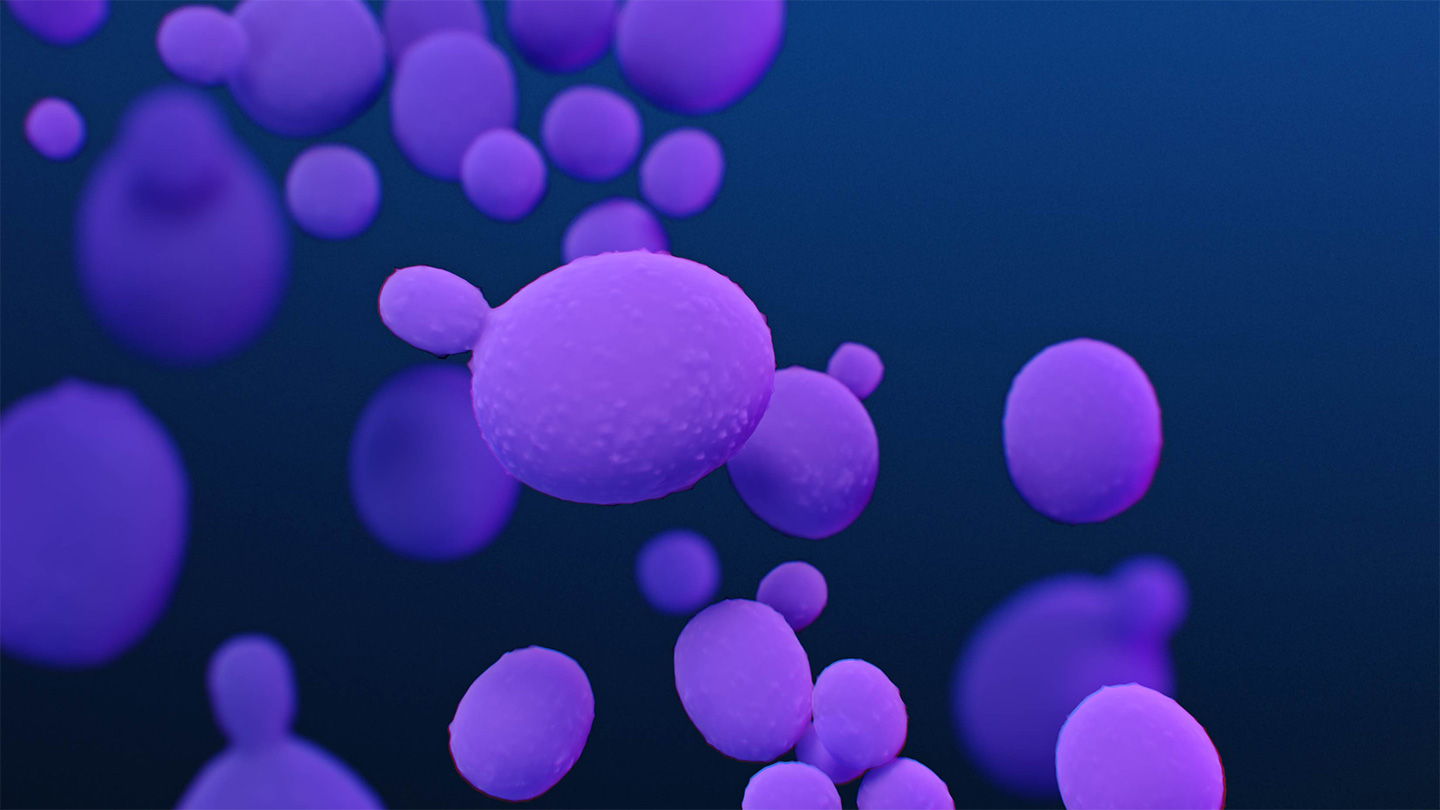
A fungus that recently evolved to infect humans is spreading rapidly in health care facilities in the United States and becoming harder to treat, a study from the U.S. Centers for Disease Control and Prevention finds.
Candida auris infections were first detected in the United States in 2013. Each year since, the number of people of infected — though still small — has increased dramatically. In 2016, the fungus sickened 53 people. In 2021, the deadly fungus infected 1,471 people, nearly twice the 756 cases from the year before, researchers report March 21 in Annals of Internal Medicine. What’s more, the team found, the fungus is becoming resistant to antifungal drugs.
Science News headlines, in your inbox
Headlines and summaries of the latest Science News articles, delivered to your email inbox every Thursday.
Thank you for signing up!
There was a problem signing you up.
The rise of cases and antifungal resistance is “concerning,” says microbiologist and immunologist Arturo Casadevall, who studies fungal infections. “You worry because [the study] is telling you what could be a harbinger of things to come.” Casadevall, of Johns Hopkins Bloomberg School of Public Health, was not involved in the CDC study.
In tests of people at high risk of infection, researchers also found 4,041 individuals who carried the fungus in 2021 but were not sick at the time. A small percentage of carriers may later get sick from the fungus, says Meghan Lyman, a medical epidemiologist in the CDC’s Mycotic Diseases Branch in Atlanta, possibly developing bloodstream infections that carry a high risk of death.
Starting in 2012, C. auris infections popped up suddenly in hospitals on three continents, probably evolving to grow at human body temperature as a result of climate change (SN: 7/26/19). The fungus, typically detected through blood or urine tests, usually infects people in health care settings such as hospitals, rehabilitation facilities and long-term care homes. Because people who get infected are often already sick, it can be hard to tell whether symptoms such as fevers are from the existing illness or an infection.
Those most at risk of infection include people who are ill; those who have catheters, breathing or feeding tubes or other invasive medical devices; and those who have repeated or long stays in health care facilities. Healthy people are usually not infected but can spread the fungus to others by contact with contaminated surfaces, including gowns and gloves worn by health care workers, Lyman says.
Growing drug resistance
Infections can be treated with antifungal drugs. But Lyman and colleagues found that the fungus is becoming resistant to an important class of such medications called echinocandins. These drugs are used as both the first line and the last line of defense against C. auris, says Casadevall.
Before 2020, six people were known to have echinocandin-resistant infections and four other people had infections resistant to all three class of existing antifungal drugs. That resistance developed during treatment using echinocandin. None of those cases passed the resistant strain to others. But in 2021, 19 people were diagnosed with echinocandin-resistant infections and seven with infections resistant to multiple drugs.
More concerning, one outbreak in Washington, D.C., and another in Texas suggested people could transmit the drug-resistant infections to each other. “Patients who had never been on echinocandins were getting these resistant strains,” Lyman says.
Some health care facilities have been able to identify cases early and prevent outbreaks. “We’re obviously very concerned,” Lyman says, “but we are encouraged by these facilities that have had success at containing it.” Using those facilities’ infection control measures may help limit cases of C. auris, she says, as well as reducing spread other fungal, bacterial and viral pathogens.