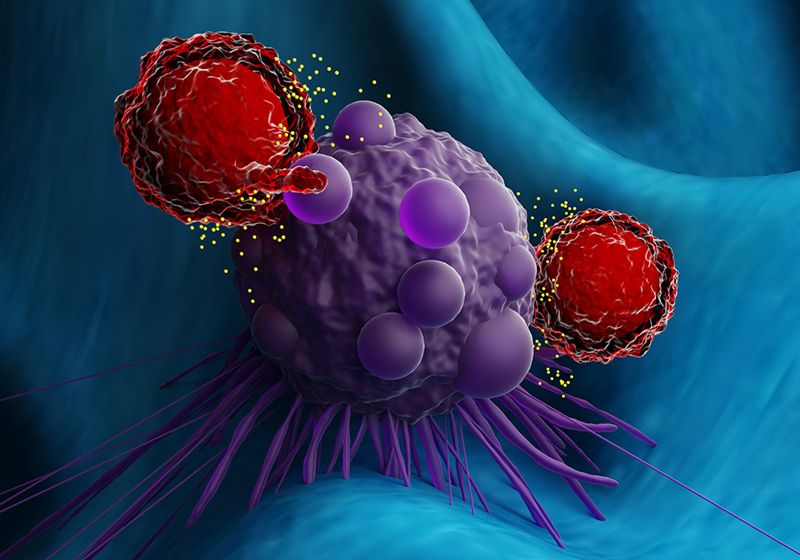
Research on adoptive cell therapies—where scientists genetically engineer a patient’s own immune cells to target the cell type that causes their symptoms—has led to incredible therapeutic successes in treating liquid tumors, but similar efforts for treating solid tumors have proved less fruitful. A key factor that limits therapeutic efficacy for solid cancers is ensuring that the engineered T cells find their way to the tumor microenvironment, a process called T cell homing. To study how T cells move through the circulation and home to a tumor, Susan Thomas, associate professor at Georgia Institute of Technology, developed a microfluidic device that mimics the tumor vasculature.1 Thomas and her team used this device to screen engineered T cells, such as CAR T cells, to find those that could reach solid tumors more effectively in vivo.
How do you model T cell homing outside of the body?
We engineered a microfluidic chip that models the vasculature in the tumor. We first incorporated flow parameters that mimic what vessels within the tumor experience, which is really important to avoid false positives and understand if T cells will interact with blood vessels in the body. We then functionalized our channel and coated it with molecules that are expressed by the tumor epithelium itself. This is different from microfluidic devices that other groups have developed, which are coated with various cell types found in the tumor microenvironment. We took this reductionist approach—creating an acellular microfluidic device—because it is adaptable: we can coat it with various concentrations and combinations of molecules to truly model and study how engineered T cells home to tumors under different conditions.
See Researchers Develop a CRISPR-Based Therapy That Penetrates Solid Tumors
Why did you choose to coat your channel with P-selectin?
We tried different molecules and conditions, but focused on selectins because they mediate very fast binding events with their cognate ligands. In the context of blood vessels where cells are flowing by, such rapid interactions are critical mediators that enable initial T cell adhesion events to the vessel wall. We focused our attention on P selectin because it is expressed by the endothelium in the context of inflammation and cancer, but we are now expanding our work to look at other adhesion receptors and ligands to test how their presence alters T cell adhesion to blood vessels and homing to tumor cells.
How did you test for homing differences among engineered T cells?
We are interested in testing the devices and technologies we develop to see if they alter cellular behavior in vivo and/or improve therapeutic efficacy. Once we developed our microfluidic chip, we scaled the system so that we could capture enough cells and fractionate those that bound to the adhesion molecules in our chip from those that did not in two different tubes. We next transferred these cells into tumor-bearing mice and analyzed their behavior. What we found was really interesting: the cells that bound our microfluidic device homed more to tumors compared to cells that did not interact on the chip. We are really excited because this work demonstrates that we can use our engineered microfluidic device to model ex vivo how therapeutic T cells home to tumors in the body.
This will allow us to optimize cell engineering protocols and improve adoptive cell therapy.”
—Susan Thomas, Georgia Institute of Technology.
What are the broader implications of this work?
Many scientists are working out different cocktails, recipes, and expansion protocols to improve the efficiency of engineered T cells prior to administering them to patients. With our microfluidic chip, we can quantify the number of cells that interact under different conditions, which allows us to directly compare how different expansion or engineering protocols for modifying immune cells for adoptive cell therapy affect the extent of adhesion and tumor homing. Because our microfluidic chip is acellular, researchers can use it to screen the final therapeutic cell product without the risk of contaminating it with exogenous materials. Our system also allows one to take that starting therapeutic cell population, even without expansion or at very early stages of expansion, and enrich for those that have increased tumor-targeting potential from the get-go, which will help reduce manufacturing time. This will allow us to optimize cell engineering protocols and improve adoptive cell therapy to have better outcomes in cancer therapy applications.
This interview has been edited for length and clarity.
References
- C.P. Carmargo et al., “Adhesion analysis via a tumor vasculature-like microfluidic device identifies CD8+ T cells with enhanced tumor homing to improve cell therapy,” Cell Rep, 42(3):112175, 2023. doi: 10.1016/j.celrep.2023.112175